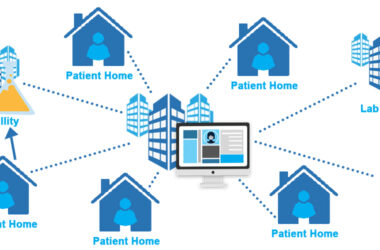
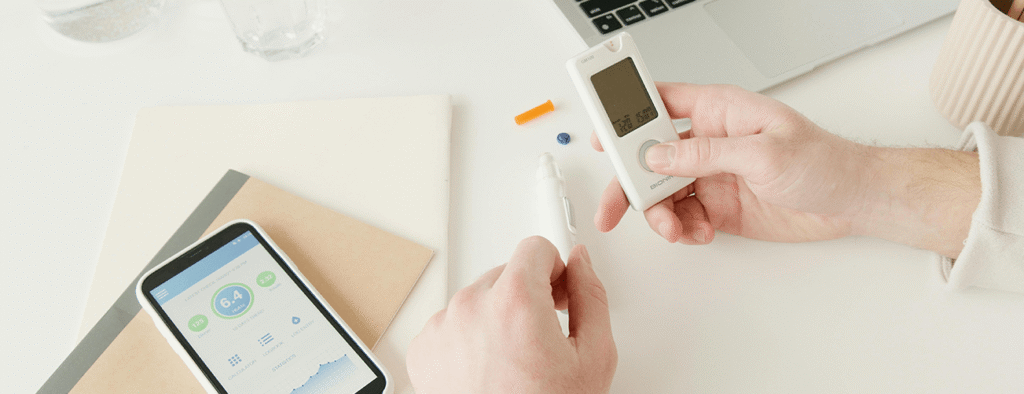
First, doctors attach small sensors to patients or ask them to wear smart patches that track their heart rate, breathing, sleep, and movement. These sensors send data over the internet so medical teams can watch health signs in real time. For example, a wireless glucose monitor can send blood sugar levels every five minutes to a nurse’s dashboard. And that constant flow of information helps care teams spot an issue before it becomes an emergency. Today more than 69 percent of health providers in the United States use at least one IoT tool for patient care, up from 34 percent in 2016.
Next, software gathers that raw data and turns it into clear graphs and alerts. When a value drifts out of the normal range, the system flags it and sends a message to a doctor or family member. This kind of alert helped cut hospital readmission for heart patients by 25 percent in a recent study. And as more teams connect sensors, databases, and apps, they build a fuller picture of each person’s health history. In that way, each patient moves from a one‑size‑fits‑all plan to a care path shaped by their own needs.
Benefits to Patients
Better Monitoring and Early Action
Patients with chronic illness find that IoT tools give them a safety net at home. When sensors record odd heart rhythms or glucose swings, an alert can trigger a nurse call or short clinic visit. That kind of early action helped lower emergency visits by 30 percent in one regional program. As a result, patients spent less time in pain and will likely avoid serious complications through quick help.
More Engagement in Health
IoT devices also give people a role in their own care. Many apps display data in simple graphs, so a person can see how sleep or diet links to blood pressure hours later. In one survey, 82 percent of users said they felt more in charge of their own health. So they stay active in simple tasks like walking and tracking fluid intake. And that steady effort adds up to stronger outcomes over months and years.
Lower Cost and Greater Access
By helping people stay well at home, IoT tools can lower health costs. One report found that connected care cut chronic disease expenses by 20 percent in a major health system (World Health Organization 2023). Remote monitoring can replace some in‑person visits with video calls or alerts, so clinics can serve more people with the same staff. That extra reach matters most in rural areas, where travel to a city hospital can take hours.
Challenges for Adoption
Data Overload and Privacy Concerns
While vast data can help, it can also overwhelm care teams. A single patient might generate millions of data points per day. Sorting that into useful alerts takes strong software and trained staff. And then comes the issue of privacy. When health data moves over the internet, it must stay secure. In 2024 alone, health data breaches affected 45 million records in the United States (HIPAA Journal). So hospitals must invest in secure networks and staff training to keep trust.
Device Costs and Patient Comfort
Some sensors cost hundreds of dollars each, and many teams must buy dozens to track a whole ward. Even though global IoT in health care rose to $72 billion in 2020 (Statista), small clinics may lack funds for top tools. Also, not every patient likes wearing a patch or carrying a device at all times. Some feel discomfort or worry about a device failing. Clinics must help people learn to use tools and set clear plans for backup in case sensors stop working.
Future Trends
Smarter Analytics and AI
Soon, health apps will learn each person’s normal data patterns and flag only new risks. This move to smart analytics will cut false alerts by 40 percent, early trials show (Frost & Sullivan 2024). And that means doctors can trust the alerts more. They can focus on patients who truly need help.
Wider Use of Wearables
Watch‑style devices now track steps and heart rate for fitness. In coming years they will gain sensors for blood oxygen, stress signals, and more. By 2025, 87 percent of hospitals will offer at least one program using patient wearables, analysts predict (IDC Health Insights 2023). That broad use will make home care part of the normal path for many conditions.
Integration with Telehealth
With more patients and doctors taking video calls, IoT data will flow into telehealth visits. A doctor will see live readings on their screen as they talk. That setup will let them make notes and adjust treatment faster. In one pilot project, this blend of video and IoT data cut virtual visit times by 15 percent, helping clinics see more patients each day (Healthcare IT News 2024).
How to Start Using IoT in Personalized Care
Assess Needs and Costs
Begin by listing the main goals for your patients. Then pick devices that fill those needs. For instance, choose continuous glucose monitors for diabetes care or cuffless blood pressure sensors for heart patients. And weigh the device cost against your budget.
Build Secure Networks
Set up encrypted channels before you add sensors. Use password rules and multi‑factor checks so only staff can see live data. Then map out how alerts will flow from sensors to care teams.
Train Staff and Patients
Offer simple guides and practice sessions. Show patients how to wear sensors and use apps. And teach staff to set safe alert limits and check data daily.
Measure Outcomes and Improve
Track key numbers such as readmission rates, call‑in volume, and patient satisfaction scores. Then adjust your tool set as you learn which devices users like and which alerts help most.
Conclusion
IoT devices bring medicine to each person’s door. They make care more precise, lower costs, and let people play an active part in their own health. And though they add work in data checks and security, the gains in fewer hospital stays and quicker help can far outweigh those costs. As sensor tools grow smarter and easier to use, they will shape how every clinic, big or small, delivers years ahead.