The digital health products continue transforming how individuals measure and manage health. And this growth is not by any means abating. With 2025 ahead, the following are the key trends that will define the way in which individuals will use technology to keep healthy and how care will be given out by providers.
Telehealth Grows into Everyday Care
This happened within a few years as telehealth, which was once a nice addition to medicine, became an essential part of it. Actually, the number of telehealth visits increased by 38 percent in 2020 when the pandemic started, and by 2024, over 50 percent of doctors introduced video check‑ins as a regular option. Industry data show that there will be about 60 percent of primary care that incorporates some sort of virtual visit by 2025. Patients can easily make a quick call than to drive to an office, and doctors can serve many people in rural locations in this manner.
When it comes to video visits, patient satisfaction is 85 percent and is equal to face-to-face care during simple checkups. And wait times decrease as much as 30 percent as appointments can fit more conveniently in the rotation of a doctor. Cost obstacles will be reduced even more as more insurers include full coverage of telehealth. This ought to drive telehealth into an even wider stage of regular visits and follow ups.
Smart Wearables Become Health Monitors
Wearable devices moved past fitness now. They track heart rate, blood sugar, sleep stages and stress levels in real time. The market for wearables reached 490 million units in shipments by 2024 and could top 540 million by 2025. That jump reflects both lower prices and higher demand for health data.
Many new devices work without a phone nearby and send alerts when numbers hit risky levels. For example a smartwatch may warn a user of a fast heartbeat pattern and suggest they seek help, cutting response time when minutes count. Data from these gadgets also help doctors spot long‑term trends in blood pressure or activity, and offer tailored tips.
People trust wearables enough that 70 percent now share data with their care team. And more products will appear that link directly to electronic health records, so a doctor sees readings in near real time. That link can cut down on paperwork and make checkups more focused on solutions.
Mobile Apps Move Past Step Counters
Apps for health started by counting steps and logging calories. Now they offer guided breathing sessions, mental health check‑ins and video lessons for physical therapy. In 2023 users downloaded over 3.4 billion health and fitness apps, up 12 percent from 2022. App makers add features that let users set goals with a coach or join small support groups, which boosts success rates by up to 25 percent.
Many apps pair with wearables or home monitors so they can log blood pressure or blood sugar without manual entry. And some include AI tools that spot patterns and send tips for improvement. For instance an app may note your sleep dips after late work nights and suggest a simple bedtime routine to help you rest better.
AI and Analytics Guide Better Choices
Artificial intelligence does more than scan images. AI now reads patient notes, weighs lab results and spots risks before they get serious. By 2025 about 65 percent of hospitals will run at least one AI tool to flag early signs of conditions like sepsis or diabetic ketoacidosis. Those tools can catch problems up to 48 hours before symptoms appear.
AI also helps drug researchers sift through mountains of data in days instead of months. That saves time in finding new treatments and speeds trials by roughly 20 percent. On the consumer side apps use AI to spot mental health needs by watching tone in messages and voice cues. They then nudge users to try a relaxation exercise or get professional help.
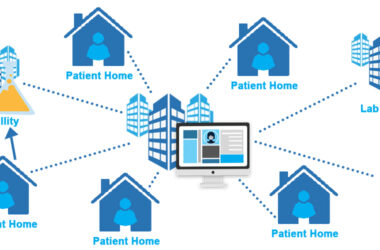
Remote Patient Monitoring Extends Care
Remote patient monitoring uses gadgets in homes to track chronic diseases. About 3.2 million patients used home monitors for blood pressure by late 2023, and that number should reach 5 million by 2025. These tools send daily updates to nurses who catch out‑of‑range readings and call the patient to adjust treatment quickly.
This model cuts hospital readmissions by around 25 percent for heart failure patients. It also gives peace of mind when problems arise at night or on weekends, and the clinic is closed. As devices get simpler to set up and insurers cover them more, many more people with long‑term conditions will manage their health from home.
Data Privacy and Security Take Center Stage
People worry that health data might leak or get sold. In response, makers of apps and devices now build in stronger safeguards. By 2025, more than 80 percent of digital health firms will use end‑to‑end encryption for data at rest and in motion. That shields information from hackers during transit and storage.
Regulators also tighten rules around consent. Many apps now require a clear yes to each type of data sharing instead of a blanket agreement buried in small print. Users can ask to see a log of who viewed their records. Those checks and balances aim to earn trust and keep data safe.
Regulatory Changes Shape the Market
Governments worked fast to allow new tools during the pandemic. By 2025, many of those temporary rules will become permanent. For exampl,e the US Food and Drug Administration will keep faster review paths for software updates that fix bugs or add low‑risk features. That means an app maker can push an update in weeks instead of months.
In Europe, new standards also demand proof of clinical benefit before a digital tool can claim to improve outcomes. That may slow some flashy releases, but it also validates what really works. Clinicians and patients will look for products that meet these strict requirements, and less effective ones will fade away over time.
What Users and Providers Should Expect
And that’s what lies ahead for digital health in 2025. People will rely more on video visits and smart gadgets for everyday needs. Apps will guide both body and mind. AI will sift data and sound alarms before both patients and doctors miss red flags. Home monitors will keep tabs on health between visits, and new rules will protect data while clearing the path for safe updates.
As these trends grow, many users will see fewer trips to the clinic just to check simple numbers and more time spent on care plans built around real‑time data. And providers will turn that same data into clearer insights and faster fixes. The result should be a system that is more patient‑friendly, more efficient, and more focused on preventing problems rather than just treating them.